Diagnostics and Stem Cell-based Treatment for Osteoarthritis - OA:
Treat the Disease, not the Symptoms
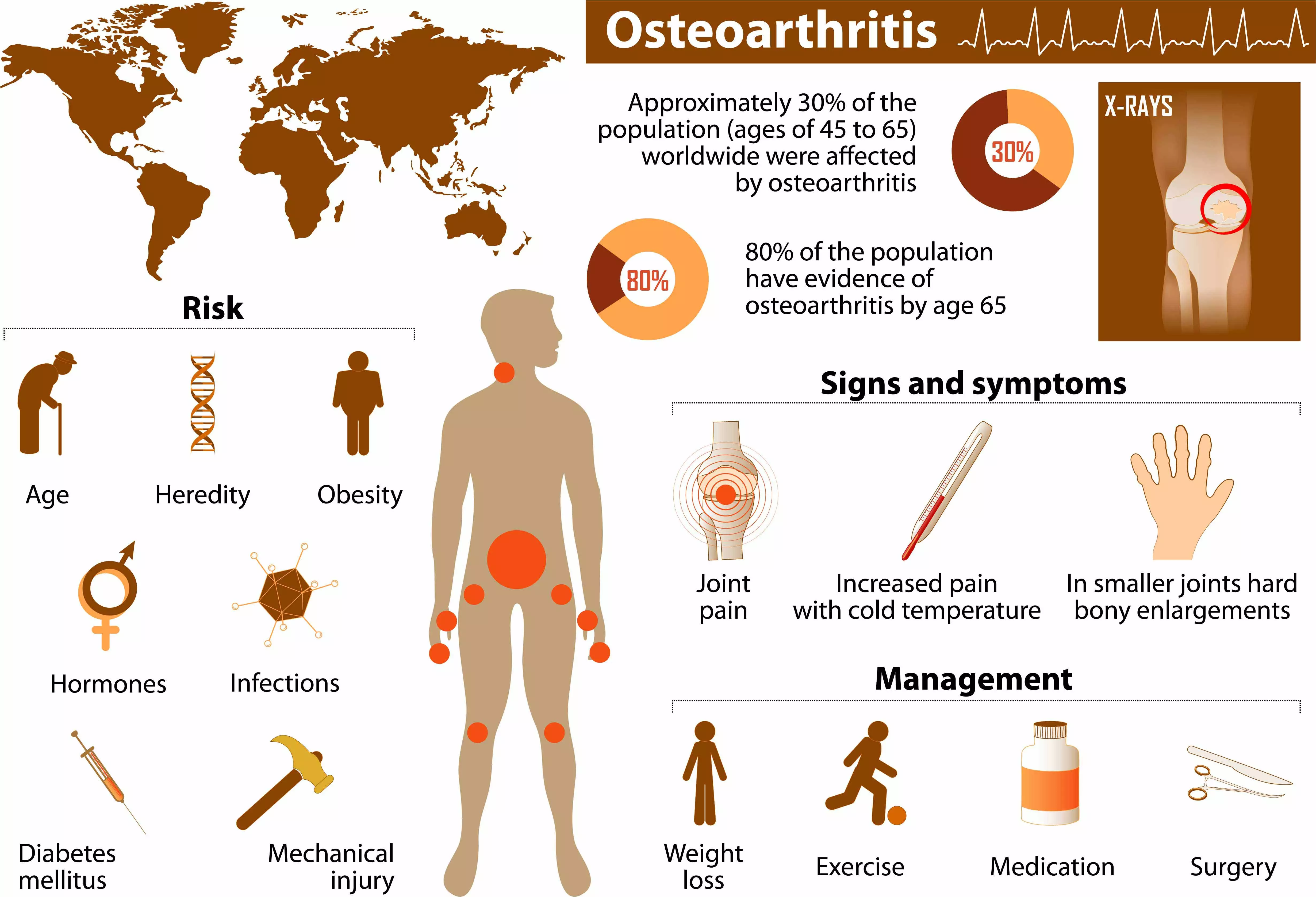
Osteoarthritis (OA) - the wear and tear of joints - affects everybody sooner or later. Arthritic joint changes are detectable in 80% of 65-year-olds; 60% suffer from symptoms. Osteoarthritis is caused by degenerative changes of the articular cartilage and underlying bone, two of the major components of joints. Inflammation of the synovial membrane, the inner lining of the joint, also play an important role during the degeneration process. The main symptoms are joint pain, limited motor function and stiffness. Osteoarthritis often affects the joints of hands, feet, spine and knees. The main risk factors are genetic, but obesity, joint injuries, lack of exercise and imbalanced sex hormones also play a role. Current therapies are mainly targeting the symptoms, however, none are able to structurally modify the processes of OA or prevent the disease's progression.
Stem cell therapies have yielded impressive results in regenerating damaged tissues and the underlying aging and immunologically-related processes of osteoarthritis. Recent evidence-based scientific research has shown that stem cell-based therapies have the potential to modulate the immune responses of OA, regenerate lost nerve supply, and regenerate other tissues.
ANOVA offers the well-studied BMC (bone marrow concentrate) as a direct injection into damaged joints as well as a novel stem cell-based therapy, the ANOVA Stem Cell Secretome Therapy, in combination with conventional therapeutic measures. Our aim is to treat patients with osteoarthritis to achieve their best treatment outcome. Our programs are one of a kind in Europe.
Stem cell therapies are still viewed as experimental treatments. But ongoing external studies, e.g. at Mayo clinic, show good patient-individual results.
For more information about our stem cell-based treatments for osteoarthritis in Germany, schedule and appointment for a consultation today.
Osteoarthritis - Diagnostics - Treatment - Stem cells - Medication
On this page we inform you about Osteoarthritis covering an overview on important aspects of causes, treatment options, precision diagnostics that reveals the cause of pain and location of the pain-causing defect, as well as our stem cell-based therapies that we offer in Offenbach (near Frankfurt/Main) Germany.
Jump directly to the following topics:
- Conventional therapies
- ANOVA therapies for OA
- Expectations and limits
- Avoid joint replacement
- Our osteoarthritis treatment
- Diagnostics of pain-causing defects
- The ANOVA difference: targeted treatment
- You want a second opinion
- Workflow of the treatment process
- Other important therapeutic possibilities
- FAQ- frequently-asked questions
- Sources and Literature
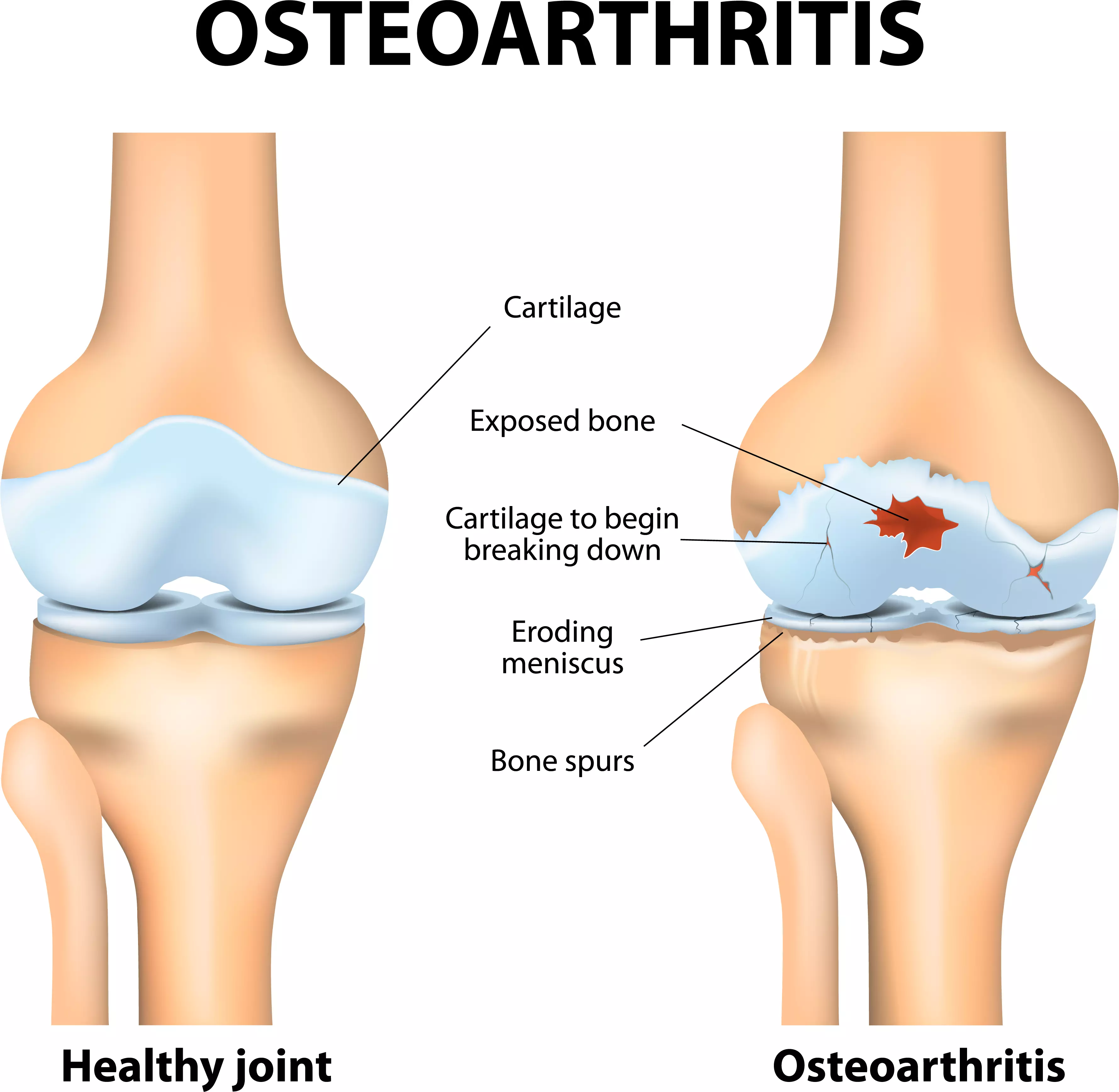
Joint and cartilage degeneration in OA
ANOVA IRM - Germany
Generally Available Conventional Therapies
Established therapies for osteoarthritis are aimed at reducing pain, and ideally at slowing down degenerative changes. Oral anti-inflammatory and pain medications such as acetaminophen, non-steroidal anti-inflammatory drugs, and weak opioid analogues can relieve symptoms in the early stages of osteoarthritis (iv). Whilst classic anti-inflammatory drugs (NSAIDs - non-steroidal anti-inflammatory drugs), such as ibu-profen, cause damage to the stomach and kidneys, the so-called COX2 inhibitors have since been largely withdrawn from the market because of an increased risk of heart attack and stroke.
Injection Therapies are commonly used in patients with unsatisfactory response to the above mentioned oral therapies. The intra-articular injection of corticosteroids is still widely used today (v, vi). However, their effect usually does not last longer than 4 weeks (vii). Although the injection of cortisone preparations into the inflamed joints results in rapid pain relief, it accelerates joint wear by damaging the cartilage cells, which are essential for the maintenance of articular cartilage.
Synthetic hyaluronic acid (HA), whose natural form is part of the synovial fluid, has been used for decades to aid the viscosity of the joint and suppress inflammation. While previous meta-analyses considered HA superior to cortisone injections, this effect could not be addressed in a recent large-scale meta-analysis (viii).
Therefore, while medication may help relief the symptoms, they may cause severe side effects that can still heavily impact the quality of life of the patients.
Stem Cell Treatments for Osteoarthritis - OA at
ANOVA Institute for Regenerative Medicine - Offenbach, Germany
BMC, Secretome/Exosomes, PRP
Potency Hypothesis of Stem Cell Therapies
Stem cells possess the potential to communicate with the immune cells that elicit the inflammation and by natural, so far not understood mechanisms may inhibit this immune-over-reaction. Furthermore, stem cells have the ability to stimulate regeneration of tissue thereby counteracting the wear and loss of cartilage in the affected joints. Negative long-term effects similar to cortisone are not expected. The aim of a stem cell treatment is therefore, the fast relief of pain, the slowing of the disease progression and in the best cases to even support joint regeneration. This can dramatically increase the quality of life, especially for patients with severe pain, as well as the movement duration and range.
Is it Possible to Relieve Pain and Avoid Joint Replacement?
Yes, there are different innovative (experimental) treatment concepts which specifically target cartilage defects with stem cell therapies and help to avoid joint replacement also in the long term. A surgical joint replacement requires long-lasting rehabilitation and often offers only moderate treatment success. Patients often re-acquire their strength and mobility after months but fail to improve their level of activity. Additionally joint implants have to be replaced regularly which results in several surgical interferences over the years for younger patients.
A specific, well-tailored stem cell therapy in contrast could postpone the surgical procedure and might even help to avoid joint replacement. For this, autologous (patient's own) stem cells are used to halt inflammation and initiate the body's own regeneration and repair system. New evidence-based external scientific and clinical studies have shown that stem cell-based therapies are able to modulate immune responses in OA and to stimulate regenerative processes in osteoarthritis by e.g. stimulation of chondrocyte replacement (the cells that produce cartilage).

Avoid joint replacement surgery
ANOVA IRM - Germany
Two Targeted Effects: Pain Relief and Progression Improvement
A stem cell treatment can elicit two effects in affected joints that build on one another. Due to the modulation of the underlying immune reaction the stem cell injection decreases or even stops the inflammation. As inflammation, especially in early stages, often is the main cause of pain, targeted stem cell injection often results in immediate pain relief up to complete pain-free movements of the treated joint.
The effects on disease progression builds on the inhibition of inflammation. Upon the halting of the inflammation the joint returns to a resting-phase and cartilage loss is reduced or stops. With adequate on-going therapy in combination with e.g. physiotherapy, regeneration of cartilage and formation of new cartilage can take place. As all effects are patient- and disease stage-dependent and may be influenced by additional, external factors, we always apply individual treatment plans. In general, pain is relieved, inflammation is reduced, further degradation and wear of the joints is slowed up to cartilage re-building.
BMC - Bone Marrow Concentrate - Autologous
Autologous (self) BMC are our main therapy option for locally-restricted Osteoarthritis especially when only the hip (Coxarthrosis), the elbow or the knee (Gonarthrosis) is affected.
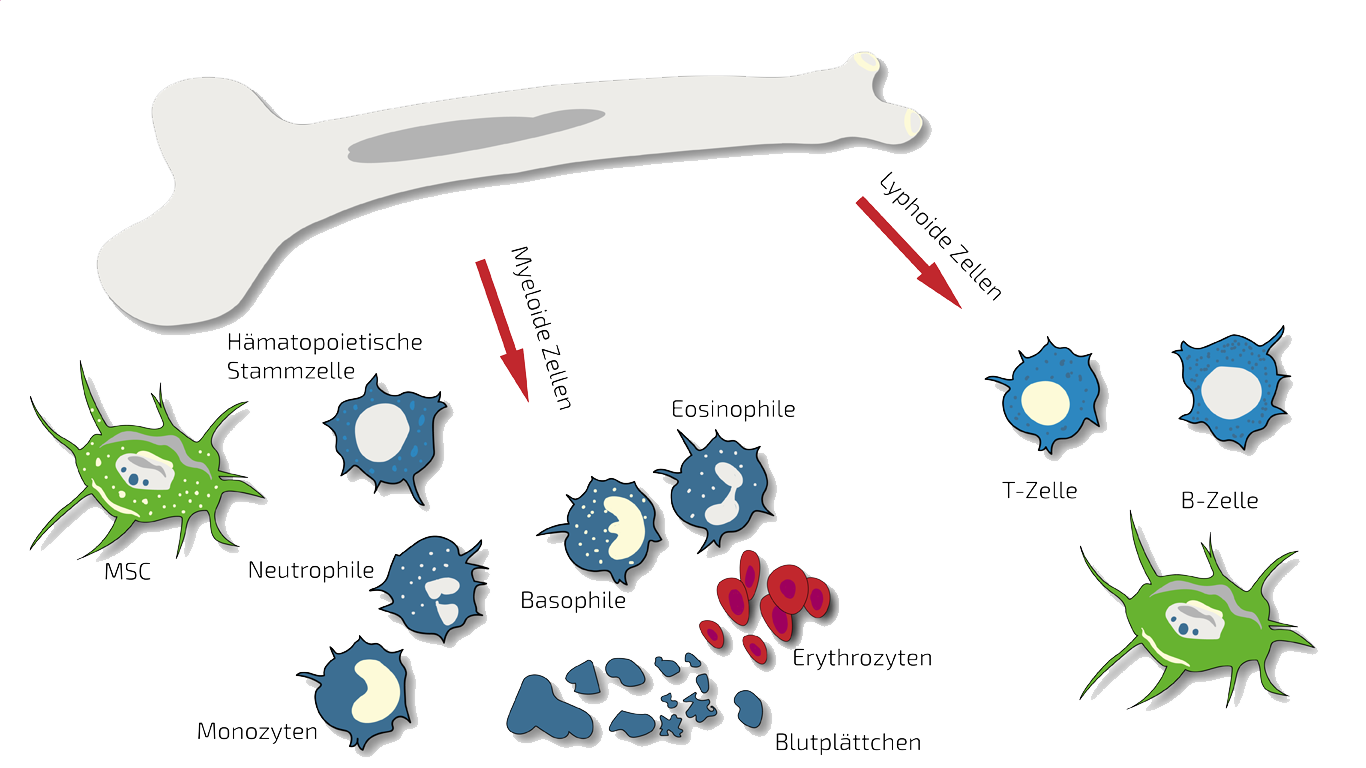
In such cases we treat specifically this joint or these joints with targeted, localized BMC injections. BMC contains autologous meaning patients own, adult stem cells (hematopoietic and mesenchymal stem cells in natural composition) which we isolate and concentrate from your pelvis crest in a short process under slight sedation.
These stem cells are supposed to inhibit the inflammation thereby relieving you from pain and to stimulate regeneration of the joint cartilage. For an on-going therapy, we combine BMC with PRP (platelet-rich plasma) or Hyaluronic Acid (see below). More information about this type of stem cell therapy is summarized on our page an BMC.
PRP - Platelet-Rich Plasma - Autologous
PRP is a comparably inexpensive experimental therapy as platelets (thrombocytes naturally containing growth factors and stimulants) are isolated from autologous (own) blood without isolation of stem cells. For Osteoarthritis, we use PRP often in combination with BMC and is administered in-between BMC treatments to continuously support the anti-inflammatory effect. Besides this, PRP is well-known as a stimulant for wound healing in e.g. periodontitis therapy or as a measure against hair loss. More on PRP (as a combination therapy) is summarized on our PRP overview page.
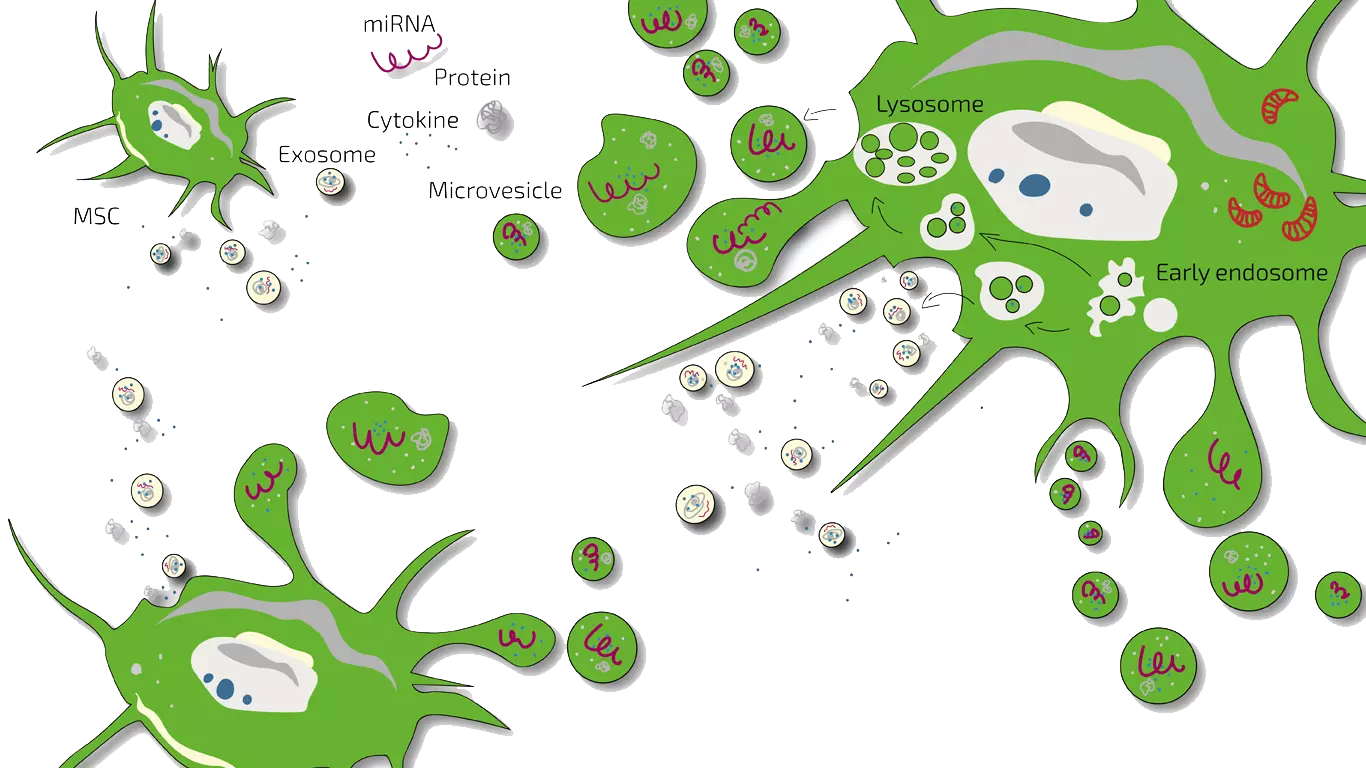
MSEC - Mesenchymal Stem Cell Secretome - Exosomes - Autologous
Preventive and as a support of BMC especially for Poly-arthritis we treat OA patients with MSEC (secretome, exosomen, EVs) of mesenchymal stem cells (MSC, AD-MSC, adipose-derived, fat-derived stem cells) which we harvest from the patients belly in a mini-liposuction (very brief and limited liposuction) under slight sedation. Worldwide, ANOVA is the first stem cell clinic to acquire legal permission form the responsible governmental authorities and therefore, offers high quality, safe and legally-controlled autologous (own) exosome-containing secretome.
The main advantage of MSEC is that in contrast to live stem cells which would loose their therapeutic potency, can be frozen without loss of exosomes. This enables us to produce 10-20 injection doses from one liposuction which can then be administered over a longer treatment period. This is especially advantageous for serious cases of wide-spread poly-arthritis. What a Secretome/Exosome is and how they compare is explained on our overview page.
Please note that this treatment is not a cure but as any stem cell treatment an experimental, potentially disease-modifying therapy. It requires regular and repeated travelling to Offenbach, Germany.
Hyaluronic Acid - HA
Another, cost efficient supportive treatment is injection of hyaluronic acid into affected joints.
Especially in early cases, this can reduce pain and result in a better "lubrication" of the joints. Bone parts do not crunch directly on another after HA injection.
Hyaluronic acid alone, on the other hand, is not expected to have regenerative effects on the damaged cartilage or bone.
Therefore, we usually combine HA with BMC treatment and HA is given intermittently between BMC treatments.
Hyaluronic acid - HA
ANOVA IRM - Germany
Contraindications
Our stem cell treatments are experimental, but we only treat patients for whom we believe the risk/benefit ratio indicates treatment based on the state of the art, i.e., medical, scientific evidence.
Please understand that we therefore do not treat patients for whom the following points apply:
- Active cancer in the last two years
- Not yet of legal age
- Existing pregnancy or lactation period
- Unable to breathe on own, ventilator
- Difficulty breathing in supine position
- Dysphagia (extreme difficulty swallowing)
- Psychiatric disorder
- Active infectious disease (Hepatitis A, B, C, HIV, Syphilis, or other)
Therapy Workflow for Osteoarthritis
The precise workflow is described in detail on the stem cell- specific pages of BMC (most often used for OA), Secretome/Exosomes and PRP (as combination therapy).
All therapies are divided into phases such as evaluation of the medical history (we analyze your current therapies and medical records), initial counseling and evaluation of potential, patient-individual benefit of a stem cell therapy (indication statement), preliminary examinations, diagnostics, consultation on all therapy options, preparation of an individual treatment plan including cost estimate, harvesting of tissue, production of the stem cell product, quality control of the product and application. There are two special features for osteoarthritis and arthritis patients. If your previous findings have not found the specific causes of your joint pain, we will examine you in advance with a precise and informative arthro-MRI or an MRI with non-radioactive contrast medium, if you wish. In addition, we often apply the stem cells (BMC) intra-articularly (i.e., directly in the joint). This means that we deliver the stem cells to the exact location where your pain originates.
Unfortunately, according to the risk-benefit ratio, we cannot treat children or pregnant women. In addition, other factors can also be exclusion criteria.
How Long Does a Stem Cell Therapy Take?
The initial analyses and counseling can be done without you having to travel to Offenbach (near Frankfurt/Main, Germany). This period can be 2 weeks up to months depending on the availability of patients slots. If you live further away, we will conduct the initial discussions by telephone or video conference. For the actual treatment, you will travel to Offenbach. Then, depending on the therapy, the tissue collection, quality control and treatment type it will take as follows:
BMC- and PRP-therapy
Each donation and application of BMC (most often used for OA) and PRP (as combination therapy) on-site period: 2 days (consecutive days).
Secretome/Exosome-therapy:
Preparation and harvest of the fat (mini-liposuction) need once 2 days (consecutive days) in Offenbach, followed by enrichment of the mesenchymal stem cells (Secretome/Exosome) and quality control. Approximately 4 weeks after the isolation, the therapy begins according to the therapy plan determined with you. You will then come to Offenbach am Main (Germany) several times for the application. The shelf life of the secretome (exosomes) is 2 years.
How Much Does Stem Cell Treatment Cost?
Our treatments are always tailored to your specific situation, disease, stage and other factors. The therapies differ in the product used (BMC, secretome, PRP or hyaluronic acid), the frequency of treatment as well as the further examinations and your sedation and anesthesia wishes. A treatment for osteoarthritis and arthritis can cost from a few hundred to several thousand euros. You will receive a cost estimate for all treatments in advance so that you can accurately estimate what a treatment would cost in your individual case.
Does my Health Insurance Cover the Therapy Costs?
Unfortunately, at the moment it is assumed that health insurance companies do not cover the costs of experimental therapies (BMC, secretome, PRP, micro-fracture technique), i.e. you will have to bear the costs entirely yourself.
How Does the ANOVA Therapy Differ?
Diagnostics – We Look for the Cause of Your Pain
Dr. mult. Michael K. Stehling, the founder of ANOVA IRM and the Vitus Prostate Center , is a radiologist (MD) and holds a PhD in physics. For this reason, the ANOVA Institute for Regenerative Medicine, in cooperation with the Prof. Stehling Institute for Diagnostic Imaging located in the same building, has the capability to use special precision diagnostics such as arthro-MRI and non-radioactive contrast MRIs.
Compared to many conventional MRIs, these methods are often able to localize the pain-causing inflammation in your joints. This enables us to determine individually how patients should be treated and where the stem cells should be applied.
Furthermore, in consultation with you, we supplement our patient-specific diagnostics with specific blood tests on hormones, inflammation parameters and other factors that are important in your case, or recommend further examinations such as a preventive MRI spinal scan.
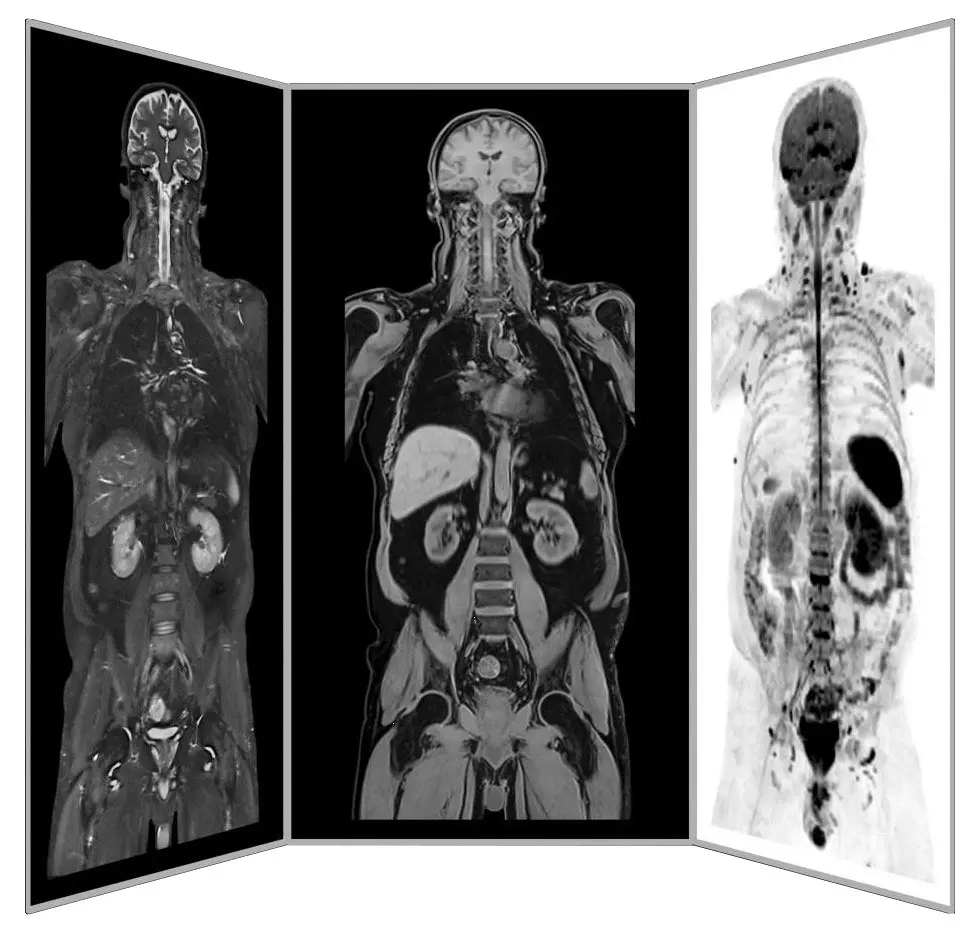
Precision MRI scans - find the source of pain
ANOVA IRM © Siemens Healthcare GmbH
How Does the ANOVA Therapy Differ?
We Implant the Stem Cells Precisely Where They are Needed
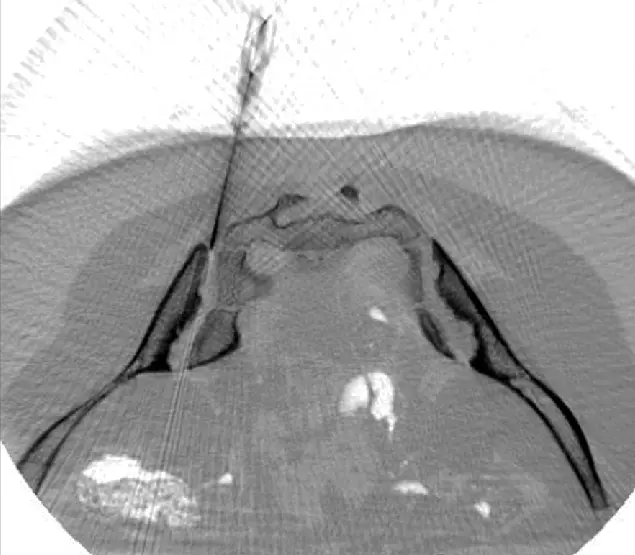
CT-assisted stem cell injection into joints
ANOVA IRM © Siemens Healthcare GmbH
Based on our specific diagnostics using arthro-MRI and non-radioactive contrast medium MRIs, we can, in contrast to many other clinics, deliver the stem cells with image support, e.g. using CT, precisely to the affected area. This means we can inject into and at joints to specifically and quickly trigger an effect where inflammation causes pain. All interventions are perfomed under supervision and care of our anesthesiologist and are pain free.
A purely intravenous administration, as many other clinics do, is only performed for the secretome (exosomes) if this is to be used additionally as a supportive or preventive measure because joint problems are present in several places in the body as the secretome is aimed to centrally modulate the immune response in order to inhibit over-reactions.
Of course, we will thoroughly advise you in the early process and the on-site consultation in advance on all steps and discuss alternatives and expectations.
Are you Interested but Uncertain?
Book a Counselling Appointment!
Our patient care managers are happy to inform you about what information we need upfront (MRI, CT, X-ray), how to transfer large data files and schedule a counseling appointment with our physicians for you. Our patient care managers are happy to inform you about what information we need upfront, how to transfer large data files and schedule a counseling appointment with our physicians for you. Please use our contact form to support a fast processing of your case and request.
You are also always welcome to send us an e-mail about your case. The counseling appointment may also take place per telephone or video chat if you live outside Germany. For more intense counseling or additional diagnostic evaluations you may also book an on-site appointment. We can perform needed MRI on the same day. All services rendered by our patient care team are free of charge and we inform you about all physician appointment charges up-front.

Avoid joint replacement with stem cell treatment
ANOVA IRM - Germany
Other Important Therapy Strategies for Osteoarthritis
Osteoarthritis is a chronic progressive diseases. Therefore, it is important to also combine any therapy with conventional approaches such as physiotherapy and exercise. We are happy to coordinate our treatments with your primary care physician or orthopedist at your location. In addition, we will be happy to advise you on nutritional supplements or infusion therapies that could support your treatment. Various substances are said to have an anti-inflammatory or regenerative supporting function.
Physiotherapy, Manual Therapy, Osteopathy, Insoles
Orthopedic treatment should always be given for osteoarthritis. Have a check to see if your legs are actually the same length or if you have hip mis-alignments that create a one-sided or incorrect body structure. In many cases, such as knee or hip osteoarthritis, muscles can stabilize the affected joint. Seek advice from a physical therapist. They can often show you specific stabilizing exercises that, if done regularly, can improve your range of motion. Use osteopathy or manual therapy to relieve any tightness or tension that may be present. Often such mis-alignments lead to further stress on joints.
Sports and Physical Activity
In many cases, moderate exercise has very positive influences on the course of osteoarthritis. Regular cycling is very promising for knee osteoarthritis. However, have your saddle height adjusted in advance at a bicycle store so that no incorrect positioning occurs. Swimming is also a very low-impact sport. You should mainly do crawl, backstroke or breaststroke with a floater. Here, one takes care to move the legs only up and down, as one would do in crawl swimming. Walking or Nordic walking can also have a very positive effect. However, in all cases, discuss your sport with your physiotherapist. In more advanced stages, water gymnastics may be the sport of choice.
Nutritional Supplementation and Nutrition
There are still few proven correlations here, but there are some promising approaches. A change in diet to a diet low in meat and rich in vegetables can help. Alcohol and nicotine should be avoided as they damage cartilage cells. Anti-inflammatory supplements are often discussed. These include omega-3 fatty acids, curcumin (turmeric), chondroitin sulfate, MSM, green-lipped mussel extract, hyaluronic acids, etc. for osteoarthritis.
You can also find more information on therapy approaches for osteoarthritis in our brochure.
Frequently Asked Questions: Stem Cell-based Treatments and Regenerative Therapies for Osteoarthritis
What is Osteoarthritis?
Osteoarthritis (OA) is the most common joint disease worldwide. In the mostly older affected persons, there is a progressive degradation of cartilage substance, which can cause joint pain and severely restrict mobility. In healthy joints, cartilage, a pressure-elastic supporting tissue, forms a buffer between the bones that meet. The knee joint is most frequently affected by osteoarthritis, followed by the hip joints and the wrists, but in principle osteoarthritis can damage any joint.
What Causes Osteoarthritis?
Osteoarthritis is mainly considered a cause of aging, where aging itself is a complicated process which is not entirely understood. Younger people sometimes get early osteoarthritis, primarily in the form of joint injuries or excessive strain.
Risk Factors are:
- Joint injury
- Joints that are deformed
- Genetic defects related to joint cartilage
- Stress on the joints from certain jobs or sports
- Being overweight
- Getting older
Quelle: By Jmarchn-Own work, CC BY-SA 3.0, https://commons.wikimedia.org/w/index.php?curid=95036158
What is the Difference Between Osteoarthritis and Rheumatoid Arthritis?
Rheumatoid arthritis is an autoimmune disease that causes inflammation of joints. So rheumatoid arthritis starts with inflammation, which then damages joints. Autoimmune essentially means that one's immune system attacks healthy cells because it thinks they are unhealthy. Different parts of the body can be affected at the same time (poly-arthritis). Rheumatoid arthritis is often found in the hands, wrists and feet.
Osteoarthritis, on the other hand, begins with joint wear, in the progression of which cartilage abrasion leads secondarily to inflammation. Osteoarthritis can be caused by a variety of non-autoimmune factors, including heavy stress on the joint, age, overweight (obesity), genetics, and birth defects.
Thus, although both conditions cause pain and discomfort due to inflammation of the joints, the course and cause, and therefore the drug treatment, differ. However, in both cases, stem cell products are a treatment option.
Is Osteoarthritis an Autoimmune Disease?
Osteoarthritis is not an autoimmune disease. This means that the weakening of joints and cartilage is not primarily caused by the immune system. It is only as the disease progresses that the joint damage causes an inflammatory response and the immune system then contributes to the further progression.
There are several risk factors that lead to osteoarthritis, such as age and weight (primary osteoarthritis) or overuse and improper stress (secondary osteoarthritis).
What is Rheumatoid Arthritis?
Rheumatoid arthritis is a chronic (persistent) inflammatory sub-type of rheumatism and is also called chronic poly-arthritis because the symptoms usually occur in very many joints. Rheumatoid arthritis is an auto-immune disease in which the misdirected immune system attacks the body's own cells and structures, causing chronic inflammation of the synovium. Women are affected by RA about 3 times more often than men. Overall, RA affects about 1% of all Europeans.
What is Rheumatism?
Rheumatism is not understood as one disease, but rheumatism summarizes various diseases. Rheumatism is therefore a collective term for more than 100 different so-called rheumatic diseases.
All rheumatic diseases have in common that they are painful and affect the musculoskeletal system or parts of it. The musculoskeletal system includes all 206 bones of the human body, more than 400 muscles and all joints, tendons and ligaments. In the course of rheumatism, the painful changes of the musculoskeletal system lead to movement restrictions.
What is the Difference Between Osteoporosis and Osteoarthritis?
Osteoporosis (bone loss) affects the thickness and strength of bones. This happens when, for example, estrogens are lacking in old age and therefore the activity of the bone-forming cells is reduced. Osteoporosis can also be triggered by hyperthyroidism or drugs such as cortisone (secondary osteoporosis). As osteoporosis progresses, the bone structure becomes large-pored or porous, i.e. increasingly thin overall, making the bones fragile. Consequently, this often causes bones to break easily. This disease can affect any bone in the body, but typical body parts affected include the spine, hips and wrists. Osteoarthritis, on the other hand, occurs when the cartilage or protective cushion between joints begins to thin. Symptoms do not include loss of bone mass or density, unlike osteoporosis.
Is Osteoarthritis Genetic? Is Osteoarthritis Hereditary?
According to studies published by the NCBI, genetics, or heredity, plays an important role in osteoarthritis. If osteoarthritis runs in your family, the risk of suffering from osteoarthritis later in life is estimated at 35 to 65%. However, since these are statistical probabilities, it does not mean for sure that you will develop osteoarthritis, especially if you have an active and healthy lifestyle. Evidence-based studies published by NCBI also state that the probabilities of inheriting osteoarthritis are different for different parts of the body. For example, there is a 40% chance of osteoarthritis occurring in the knees if these traits are inherited. While inheriting the osteoarthritis traits for the hips and hands has a 65% chance of leading to later disease.
Because osteoarthritis appears to have partly hereditary factors, scientists are working to learn more about the disease by analyzing genomes and bio-bank data.
Early Detection of Joint Changes can Prevent Osteoarthritis
While the concept of prevention through early detection of benign precancerous lesions, e.g. colon polyps or "carcinoma in situ" of the breast, has long been established in the case of cancer, such prevention concepts do not yet exist in the case of osteoarthritis. In expert circles, however, the concept of "pre-arthrosis" has recently been the subject of scientific discussion. With the aid of modern imaging techniques, it is possible to visualize early onset structural changes in articular cartilage and sub-chondral bone structure that indicate the onset of osteoarthritis. Magnetic resonance imaging (MRI) and optical coherence tomography (OCT) play an important role here, although OCT requires instruments to be inserted into the joint. Caught early, countermeasures can be taken: Relieving joint stress, improving bio-mechanics, exercise, hormone replacement, and therapies with cytokines and stem cells can slow down osteoarthritis.
How Does Cortisone Work?
Injection of cortisone (corticosteroids) into inflamed joints is still widely used today. It typically results in rapid pain relief, but its effects usually do not last longer than 4 weeks. However, in the long run, cortisone injections accelerate joint wear by damaging cartilage cells, which are essential for maintaining articular cartilage.
What are NSAID, NSAP, NSAR?
All these abbreviations stand for anti-inflammatory drug groups that are used for inflammatory processes and diseases such as rheumatism, osteoarthritis and arthritis. NS always stands for non-steroidal, i.e. substances that are not derived from steroids such as cortisone. All non-steroidal anti-inflammatory drugs have sometimes serious side effects such as damage to the gastrointestinal mucosa or heart and kidney damage. Some preparations have therefore been withdrawn from the market.
- NSAID - non-steroidal anti-inflammatory drug
- NSAP - non-steroidal anti-inflammatory drug
- NSAID - non-steroidal anti-inflammatory drug (translated non-steroidal anti-inflammatory drug)
What are Anti-Phlogistic Drugs?
Anti-phlogistic drugs are anti-inflammatory drugs. Anti-inflammatory drugs include the following groups of drugs:
- Glucocorticoids (e.g., cortisone).
- Non-steroidal anti-inflammatory drugs (NSAIDs, non-steroidal anti-rheumatic drugs)
- Immunosuppressants (DMARDs, disease-modifying anti-rheumatic drugs
- Certain novel biologic-derived drugs (biologicals, e.g., JAK inhibitors)
Effects, Risks and Side Effects of Drugs and Treatments
Patients are always individuals with their own history and specific disease course. Therefore, for drugs or treatments, one can generally never guarantee an effect or grant or exclude risks and side effects. Common expectations are summarized below. However, patient-specific deviations are to be expected.
When do I Need Joint Replacement
The established therapies for osteoarthritis aim to reduce pain, ideally to slow down the degenerative changes. In the end - when the pain becomes too severe with conventional treatment - the only option left so far in most cases is joint replacement with artificial joints, so-called endo-prostheses. Despite modern technology, these cannot completely replace the function of the natural joint, since even the necessary surgery damages the functional interaction of bones, muscles and tendons. In most cases, lengthy rehabilitation measures are required after the operation and sporting activities are restricted. Hip prostheses are now usually used successfully, while complications still occur frequently with knee prostheses, so that some physiotherapists advise against knee prostheses because they see greater chances of improving the patient's situation by means of physiotherapy without joint replacement. Also, the life of arthro-plasties is limited because metal and plastic are subject to constant abrasion and structural fatigue. This wear is not compensated for by remodeling and regrowth of tissue, as is the case with natural joints. Thus, many endo-prostheses have to be replaced after 10 - 20 years, which leads to even greater functional limitations.
What is Bone Marrow Concentrate - BMC?
Bone Marrow concentrate (BMC) is a source for Mesenchymal Stem Cells (MSCs) and Hematopoietic Stem cells (HSC). It contains many important growth and regenerative factors, in addition to the MSC and HSC in natural composition. The BMC procedure is relatively simple and minimally invasive, therefore it has been a favorite source for stem cell-based therapies in the previous decades. Many clinics rely on BMC as their main stem cell treatment, sometimes with exaggerated claims. However, BMC has demonstrated impressive results for effective treatment of numerous diseases, among them being osteoarthritis. Read more about our BMC Treatment here.
What is Platelet Rich Plasma - PRP?
Platelet Rich Plasma (PRP) is a blood-derived, cellular product with concentrated supply of regenerative growth factors and cytokines, obtained from the patient's own blood. It is very simple to acquire, and it has shown promising results in the treatment of several inflammatory and degenerative diseases. For the treatment of specific diseases, it can be combined with BMC or adMSCs, as it has synergistic additive effects to the treatment. PRP has "special" functions: it serves as a growth medium to maintain stem cells healthy; ensures adequate cellular environment where enough energy is provided to allow the cells to perform their regenerative work.
Is Therapeutic Success Guaranteed?
No therapy can guarantee a 100% success after treatment. However, in the case of experimental therapies such as stem cell therapy, the attending physician must perform a benefit-to-risk analysis for each patient and determine both the benefits and the risks for that particular patient. If the potential benefit outweighs the potential side effects, the doctor may recommend experimental therapy.
What are Other Treatments for Osteoarthritis?
Doctors often combine treatments that are optimized to fit a patient's needs, lifestyle, and health. Osteoarthritis treatment has four main goals
- Control of pain
- Improve joint function
- Keep a healthy body weight
- Achieve a healthy lifestyle
Osteoarthritis treatment plans can involve:
- Exercise
- Weight control and diet, such as:
- Low saturated fat, high fiber-rich foods, fruits and vegetables. Some nutrition supplements appear to be helpful.
- Rest and joint care
- Non-drug pain relief techniques to control pain
- Medication
- Complementary and alternative therapies
+49 (0) 69 50 50 00 944
References and Literature - Stem Cell-based Therapies and Osteoarthritis
- Neogi, Tuhina. “The epidemiology and impact of pain in osteoarthritis.” Osteoarthritis and Cartilage 21.9 (2013): 1145-1153.
- Goldring, Mary B., and Steven R. Goldring. “Articular cartilage and subchondral bone in the pathogenesis of osteoarthritis.” Annals of the New York Academy of Sciences 1192.1 (2010): 230-237.
- IIshiguro, Naoki, Toshihisa Kojima, and A. Robin Poole. “Mechanism of cartilage destruction in osteoarthritis.” Nagoya journal of medical science 65.3-4 (2002): 73-84.
- Jordan, K. M., et al. “EULAR Recommendations 2003: an evidence based approach to the management of knee osteoarthritis: Report of a Task Force of the Standing Committee for International Clinical Studies Including Therapeutic Trials (ESCISIT).” Annals of the rheumatic diseases 62.12 (2003): 1145-1155.
- Hameed, Farah, and Joseph Ihm. “Injectable medications for osteoarthritis.” PM&R 4.5 (2012): S75-S81.
- Cheng, Olivia T., et al. “Evidence-based knee injections for the management of arthritis.” Pain medicine 13.6 (2012): 740-753.
- Bannuru, Raveendhara R., et al. “Therapeutic trajectory of hyaluronic acid versus corticosteroids in the treatment of knee osteoarthritis: A systematic review and meta-analysis.” Arthritis Care & Research 61.12 (2009): 1704-1711.
- Rutjes, Anne WS, et al. “Viscosupplementation for osteoarthritis of the knee: a systematic review and meta-analysis.” Annals of internal medicine 157.3 (2012): 180-191.
- Braun, Hillary J., and Garry E. Gold. “Diagnosis of osteoarthritis: imaging.” Bone 51.2 (2012): 278-288.
- Ahmed, Usman, et al. “Protein oxidation, nitration and glycation biomarkers for early-stage diagnosis of osteoarthritis of the knee and typing and progression of arthritic disease.” Arthritis research & therapy 18.1 (2016): 250.
- Chen, Shaoliang, et al. “Intracoronary transplantation of autologous bone marrow mesenchymal stem cells for ischemic cardiomyopathy due to isolated chronic occluded left anterior descending artery.” The Journal of invasive cardiology 18.11 (2006): 552-556.
- Bang, Oh Young, et al. “Autologous mesenchymal stem cell transplantation in stroke patients.” Annals of Neurology: Official Journal of the American Neurological Association and the Child Neurology Society 57.6 (2005): 874-882.
- Pal, Rakhi, et al. “Ex vivo-expanded autologous bone marrow-derived mesenchymal stromal cells in human spinal cord injury/paraplegia: a pilot clinical study.” Cytotherapy 11.7 (2009): 897-911.
- Venkataramana, Neelam K., et al. “Open-labeled study of unilateral autologous bone-marrow-derived mesenchymal stem cell transplantation in Parkinson’s disease.” Translational Research 155.2 (2010): 62-70.
- Harris, Violaine K., et al. “Phase I trial of intrathecal mesenchymal stem cell-derived neural progenitors in progressive multiple sclerosis.” EBioMedicine 29 (2018): 23-30.
- Sun, Lingyun, et al. “Mesenchymal stem cell transplantation reverses multiorgan dysfunction in systemic lupus erythematosus mice and humans.” Stem cells 27.6 (2009): 1421-1432.
- Dash, Nihar Ranjan, et al. “Targeting nonhealing ulcers of lower extremity in human through autologous bone marrow-derived mesenchymal stem cells.” Rejuvenation research 12.5 (2009): 359-366.
- Wakitani, Shigeyuki, et al. “Safety of autologous bone marrow-derived mesenchymal stem cell transplantation for cartilage repair in 41 patients with 45 joints followed for up to 11 years and 5 months.” Journal of Tissue Engineering and Regenerative Medicine 5.2 (2011): 146-150.
- Khatab, S., et al. “Mesenchymal stem cell secretome reduces pain and prevents cartilage damage in a murine osteoarthritis model.” European cells & materials 36 (2018): 218-230.
- Themistocleous, George S., et al. “Effectiveness of a single intra-articular bone marrow aspirate concentrate (BMAC) injection in patients with grade 3 and 4 knee osteoarthritis.” Heliyon 4.10 (2018): e00871.
- Laver, Lior, et al. “PRP for degenerative cartilage disease: a systematic review of clinical studies.” Cartilage 8.4 (2017): 341-364.
- Mishra, Allan, James Woodall Jr, and Amy Vieira. “Treatment of tendon and muscle using platelet-rich plasma.” Clinics in sports medicine 28.1 (2009): 113-125.
- Laver, Lior, et al. “PRP for degenerative cartilage disease: a systematic review of clinical studies.” Cartilage 8.4 (2017): 341-364.
- Andia, Isabel, Mikel Sánchez, and Nicola Maffulli. “Joint pathology and platelet-rich plasma therapies.” Expert opinion on biological therapy 12.1 (2012): 7-22.
- Esposito, Marco, et al. “Effectiveness of sinus lift procedures for dental implant rehabilitation: a Cochrane systematic.” Eur J Oral Implantol 3.1 (2010): 7-26.
- Por, Yong-Chen, et al. “Use of tissue sealants in face-lifts: a metaanalysis.” Aesthetic plastic surgery 33.3 (2009): 336-339.
- Abd-Elsayed, Alaa. “Stem cells for the treatment of knee osteoarthritis: a comprehensive review.” Pain physician 21 (2018): 229-241.
- Bendinelli, Paola, et al. “Molecular basis of anti-inflammatory action of platelet-rich plasma on human chondrocytes: Mechanisms of NF-kB inhibition via HGF.” Journal of cellular physiology 225.3 (2010): 757-766.
- Murphy JM, Fink DJ, Hunziker EB, et al. Stem cell therapy in a caprine model of osteoarthritis. Arthritis Rheum. 2003;48:3464–74.
- Lee KB, Hui JH, Song IC, Ardany L, et al. Injectable mesenchymal stem cell therapy for large cartilage defects—a porcine model. Stem Cell. 2007;25:2964–71.
- Saw KY, Hussin P, Loke SC, et al. Articular cartilage regeneration with autologous marrow aspirate and hyaluronic acid: an experimental study in a goat model. Arthroscopy. 2009;25(12):1391–400.
- Black L, Gaynor J, Adams C, et al. Effect of intra-articular injection of autologous adipose-derived mesenchymal stem and regenerative cells on clinical signs of chronic osteoarthritis of the elbow joint in dogs. Vet Ther. 2008;9:192-200.
- Centeno C, Busse D, Kisiday J, et al. Increased knee cartilage volume in degenerative joint disease using percutaneously implanted, autologous mesenchymal stem cells. Pain Physician. 2008;11(3):343–53.
- Centeno C, Kisiday J, Freeman M, et al. Partial regeneration of the human hip via autologous bone marrow nucleated cell transfer: a case study. Pain Physician. 2006;9:253–6.
- Centeno C, Schultz J, Cheever M. Safety and complications reporting on the re-implantation of culture-expanded mesenchymal stem cells using autologous platelet lysate technique. Curr Stem Cell. 2011;5(1):81–93.
- Pak J. Regeneration of human bones in hip osteonecrosis and human cartilage in knee osteoarthritis with autologous adipose derived stem cells: a case series. J Med Case Rep. 2001;5:296.
- Kuroda R, Ishida K, et al. Treatment of a full-thickness articular cartilage defect in the femoral condyle of an athlete with autologous bone-marrow stromal cells. Osteoarthritis Cartilage. 2007;15:226–31.
- Emadedin M, Aghdami N, Taghiyar L, et al. Intra-articular injection of autologous mesenchymal stem cells in six patients with knee osteoarthritis. Arch Iran Med. 2012;15(7):422–8.
- Saw KY et al. Articular cartilage regeneration with autologous peripheral blood stem cells versus hyaluronic acid: a randomized controlled trial. Arthroscopy. 2013;29(4):684–94.
- Vangsness CT, Farr J, Boyd J, et al. Adult human mesenchymal stem cells delivered via intra-articular injection to the knee following partial medial meniscectomy. J Bone Joint Surg. 2014;96(2):90–8.
- Freitag, Julien, et al. "Mesenchymal stem cell therapy in the treatment of osteoarthritis: reparative pathways, safety and efficacy–a review." BMC musculoskeletal disorders 17.1 (2016): 230.
- Maumus, Marie, Christian Jorgensen, and Danièle Noël. "Mesenchymal stem cells in regenerative medicine applied to rheumatic diseases: role of secretome and exosomes." Biochimie 95.12 (2013): 2229-2234.
- Dostert, Gabriel, et al. "How do mesenchymal stem cells influence or are influenced by microenvironment through extracellular vesicles communication?." Frontiers in Cell and Developmental Biology 5 (2017).
- Dostert, Gabriel, et al. "How do mesenchymal stem cells influence or are influenced by microenvironment through extracellular vesicles communication?." Frontiers in Cell and Developmental Biology 5 (2017).
- Chaparro, Orlando, and Itali Linero. "Regenerative Medicine: A New Paradigm in Bone Regeneration." (2016).
- Toh, Wei Seong, et al. "MSC exosome as a cell-free MSC therapy for cartilage regeneration: Implications for osteoarthritis treatment." Seminars in Cell & Developmental Biology. Academic Press, 2016.
- Chaparro, Orlando, and Itali Linero. "Regenerative Medicine: A New Paradigm in Bone Regeneration." (2016).
- S. Koelling, J. Kruegel, M. Irmer, J.R. Path, B. Sadowski, X. Miro, et al., Migratory chondrogenic progenitor cells from repair tissue during the later stages of human osteoarthritis, Cell Stem Cell 4 (2009) 324–335.
- B.A. Jones, M. Pei, Synovium-Derived stem cells: a tissue-Specific stem cell for cartilage engineering and regeneration, Tissue Eng. B: Rev. 18 (2012) 301–311.
- W. Ando, J.J. Kutcher, R. Krawetz, A. Sen, N. Nakamura, C.B. Frank, et al., Clonal analysis of synovial fluid stem cells to characterize and identify stable mesenchymal stromal cell/mesenchymal progenitor cell phenotypes in a porcine model: a cell source with enhanced commitment to the chondrogenic lineage, Cytotherapy 16 (2014) 776–788.
- K.B.L. Lee, J.H.P. Hui, I.C. Song, L. Ardany, E.H. Lee, Injectable mesenchymal stem cell therapy for large cartilage defects—a porcine model, Stem Cells 25 (2007) 2964–2971.
- W.-L. Fu, C.-Y. Zhou, J.-K. Yu, A new source of mesenchymal stem cells for articular cartilage repair: mSCs derived from mobilized peripheral blood share similar biological characteristics in vitro and chondrogenesis in vivo as MSCs from bone marrow in a rabbit model, Am. J. Sports Med. 42 (2014) 592–601.
- X. Xie, Y. Wang, C. Zhao, S. Guo, S. Liu, W. Jia, et al., Comparative evaluation of MSCs from bone marrow and adipose tissue seeded in PRP-derived scaffold for cartilage regeneration, Biomaterials 33 (2012) 7008–7018.
- E.-R. Chiang, H.-L. Ma, J.-P. Wang, C.-L. Liu, T.-H. Chen, S.-C. Hung, Allogeneic mesenchymal stem cells in combination with hyaluronic acid for the treatment of osteoarthritis in rabbits, PLoS One 11 (2016) e0149835.
- H. Nejadnik, J.H. Hui, E.P. Feng Choong, B.-C. Tai, E.H. Lee, Autologous bone marrow–derived mesenchymal stem cells versus autologous chondrocyte implantation: an observational cohort study, Am. J. Sports Med. 38 (2010) 1110–1116.
- I. Sekiya, T. Muneta, M. Horie, H. Koga, Arthroscopic transplantation of synovial stem cells improves clinical outcomes in knees with cartilage defects, Clin. Orthop. Rel. Res. 473 (2015) 2316–2326.
- Y.S. Kim, Y.J. Choi, Y.G. Koh, Mesenchymal stem cell implantation in knee osteoarthritis: an assessment of the factors influencing clinical outcomes, Am. J. Sports Med. 43 (2015) 2293–2301.
- W.-L. Fu, Y.-F. Ao, X.-Y. Ke, Z.-Z. Zheng, X. Gong, D. Jiang, et al., Repair of large full-thickness cartilage defect by activating endogenous peripheral blood stem cells and autologous periosteum flap transplantation combined with patellofemoral realignment, Knee 21 (2014) 609–612.
- Y.-G. Koh, O.-R. Kwon, Y.-S. Kim, Y.-J. Choi, D.-H. Tak, Adipose-derived mesenchymal stem cells with microfracture versus microfracture alone: 2-year follow-up of a prospective randomized trial, Arthrosc. J. Arthrosc. Relat. Surg. 32 (2016) 97–109.
- T.S. de Windt, L.A. Vonk, I.C.M. Slaper-Cortenbach, M.P.H. van den Broek, R. Nizak, M.H.P. van Rijen, et al., Allogeneic mesenchymal stem cells stimulate cartilage regeneration and are safe for single-Stage cartilage repair in humans upon mixture with recycled autologous chondrons, Stem Cells (2016) (n/a-n/a).
- L. da Silva Meirelles, A.M. Fontes, D.T. Covas, A.I. Caplan, Mechanisms involved in the therapeutic properties of mesenchymal stem cells, Cytokine Growth Factor Rev. 20 (2009) 419–427.
- W.S. Toh, C.B. Foldager, M. Pei, J.H.P. Hui, Advances in mesenchymal stem cell-based strategies for cartilage repair and regeneration, Stem Cell Rev. Rep. 10 (2014) 686–696.
- R.C. Lai, F. Arslan, M.M. Lee, N.S.K. Sze, A. Choo, T.S. Chen, et al., Exosome secreted by MSC reduces myocardial ischemia/reperfusion injury, Stem Cell Res. 4 (2010) 214–222.
- S. Zhang, W.C. Chu, R.C. Lai, S.K. Lim, J.H.P. Hui, W.S. Toh, Exosomes derived from human embryonic mesenchymal stem cells promote osteochondral regeneration, Osteoarthr. Cartil. 24 (2016) 2135–2140.
- S. Zhang, W. Chu, R. Lai, J. Hui, E. Lee, S. Lim, et al., 21 – human mesenchymal stem cell-derived exosomes promote orderly cartilage regeneration in an immunocompetent rat osteochondral defect model, Cytotherapy 18 (2016) S13.
- C.T. Lim, X. Ren, M.H. Afizah, S. Tarigan-Panjaitan, Z. Yang, Y. Wu, et al., Repair of osteochondral defects with rehydrated freeze-Ddried oligo poly(ethylene glycol) fumarate] hydrogels seeded with bone marrow mesenchymal stem cells in a porcine model, Tissue Eng. A 19 (2013) 1852–1861.
- A. Gobbi, G. Karnatzikos, S.R. Sankineani, One-step surgery with multipotent stem cells for the treatment of large full-thickness chondral defects of the knee, Am. J. Sports Med. 42 (2014) 648–657.
- A. Gobbi, C. Scotti, G. Karnatzikos, A. Mudhigere, M. Castro, G.M. Peretti, One-step surgery with multipotent stem cells and Hyaluronan-based scaffold for the treatment of full-thickness chondral defects of the knee in patients older than 45 years, Knee Surg. Sports Traumatol. Arthrosc. (2016) 1–8.
- A. Gobbi, G. Karnatzikos, C. Scotti, V. Mahajan, L. Mazzucco, B. Grigolo, One-step cartilage repair with bone marrow aspirate concentrated cells and collagen matrix in full-thickness knee cartilage lesions: results at 2-Year follow-up, Cartilage 2 (2011) 286–299.
- K.L. Wong, K.B.L. Lee, B.C. Tai, P. Law, E.H. Lee, J.H.P. Hui, Injectable cultured bone marrow-derived mesenchymal stem cells in varus knees with cartilage defects undergoing high tibial osteotomy: a prospective, randomized controlled clinical trial with 2 years’ follow-up, Arthrosc. J. Arthrosc. Relat. Surg. 29 (2013) 2020–2028.
- J.M. Hare, J.E. Fishman, G. Gerstenblith, et al., Comparison of allogeneic vs autologous bone marrow–derived mesenchymal stem cells delivered by transendocardial injection in patients with ischemic cardiomyopathy: the poseidon randomized trial, JAMA 308 (2012) 2369–2379.
- L. Wu, J.C.H. Leijten, N. Georgi, J.N. Post, C.A. van Blitterswijk, M. Karperien, Trophic effects of mesenchymal stem cells increase chondrocyte proliferation and matrix formation, Tissue Eng. A 17 (2011) 1425–1436.
- L. Wu, H.-J. Prins, M.N. Helder, C.A. van Blitterswijk, M. Karperien, Trophic effects of mesenchymal stem cells in chondrocyte Co-Cultures are independent of culture conditions and cell sources, Tissue Eng. A 18 (2012) 1542–1551.
- S.K. Sze, D.P.V. de Kleijn, R.C. Lai, E. Khia Way Tan, H. Zhao, K.S. Yeo, et al., Elucidating the secretion proteome of human embryonic stem cell-derived mesenchymal stem cells, Mol. Cell. Proteomics 6 (2007) 1680–1689.
- M.B. Murphy, K. Moncivais, A.I. Caplan, Mesenchymal stem cells: environmentally responsive therapeutics for regenerative medicine, Exp. Mol. Med. 45 (2013) e54.
- M.J. Lee, J. Kim, M.Y. Kim, Y.-S. Bae, S.H. Ryu, T.G. Lee, et al., Proteomic analysis of tumor necrosis factor--induced secretome of human adipose tissue-derived mesenchymal stem cells, J. Proteome Res. 9 (2010) 1754–1762.
- S. Bruno, C. Grange, M.C. Deregibus, R.A. Calogero, S. Saviozzi, F. Collino, et al., Mesenchymal stem cell-derived microvesicles protect against acute tubular injury, J. Am. Soc. Nephrol. 20 (2009) 1053–1067.
- M. Yá˜nez-Mó, P.R.-M. Siljander, Z. Andreu, A.B. Zavec, F.E. Borràs, E.I. Buzas, et al. Biological properties of extracellular vesicles and their physiological functions (2015).
- C. Lawson, J.M. Vicencio, D.M. Yellon, S.M. Davidson, Microvesicles and exosomes: new players in metabolic and cardiovascular disease, J. Endocrinol. 228 (2016) R57–R71.
- A.G. Thompson, E. Gray, S.M. Heman-Ackah, I. Mager, K. Talbot, S.E. Andaloussi, et al., Extracellular vesicles in neurodegenerative diseas—pathogenesis to biomarkers, Nat. Rev. Neurol. 12 (2016) 346–357.
- I.E.M. Bank, L. Timmers, C.M. Gijsberts, Y.-N. Zhang, A. Mosterd, J.-W. Wang, et al., The diagnostic and prognostic potential of plasma extracellular vesicles for cardiovascular disease, Expert Rev. Mol. Diagn. 15 (2015) 1577–1588.
- T. Kato, S. Miyaki, H. Ishitobi, Y. Nakamura, T. Nakasa, M.K. Lotz, et al., Exosomes from IL-1 stimulated synovial fibroblasts induce osteoarthritic changes in articular chondrocytes, Arthritis. Res. Ther. 16 (2014) 1–11.
- R.W.Y. Yeo, S.K. Lim, Exosomes and their therapeutic applications, in: C. Gunther, A. Hauser, R. Huss (Eds.), Advances in Pharmaceutical Cell TherapyPrinciples of Cell-Based Biopharmaceuticals, World Scientific, Singapore, 2015, pp. 477–491.
- X. Qi, J. Zhang, H. Yuan, Z. Xu, Q. Li, X. Niu, et al., Exosomes secreted by human-Induced pluripotent stem cell-derived mesenchymal stem cells repair critical-sized bone defects through enhanced angiogenesis and osteogenesis in osteoporotic rats, Int. J. Biol. Sci. 12 (2016) 836–849.
- R.C. Lai, F. Arslan, S.S. Tan, B. Tan, A. Choo, M.M. Lee, et al., Derivation and characterization of human fetal MSCs: an alternative cell source for large-scale production of cardioprotective microparticles, J. Mol. Cell. Cardiol. 48 (2010) 1215–1224.
- Y. Zhou, H. Xu, W. Xu, B. Wang, H. Wu, Y. Tao, et al., Exosomes released by human umbilical cord mesenchymal stem cells protect against cisplatin-induced renal oxidative stress and apoptosis in vivo and in vitro, Stem Cell Res. Ther. 4 (2013) 1–13.
- Y. Qin, L. Wang, Z. Gao, G. Chen, C. Zhang, Bone marrow stromal/stem cell-derived extracellular vesicles regulate osteoblast activity and differentiation in vitro and promote bone regeneration in vivo, Sci. Rep. 6 (2016) 21961.
- M. Nakano, K. Nagaishi, N. Konari, Y. Saito, T. Chikenji, Y. Mizue, et al., Bone marrow-derived mesenchymal stem cells improve diabetes-induced cognitive impairment by exosome transfer into damaged neurons and astrocytes, Sci. Rep. 6 (2016) 24805.
- K. Nagaishi, Y. Mizue, T. Chikenji, M. Otani, M. Nakano, N. Konari, et al., Mesenchymal stem cell therapy ameliorates diabetic nephropathy via the paracrine effect of renal trophic factors including exosomes, Sci. Rep. 6 (2016) 34842.
- S.R. Baglio, K. Rooijers, D. Koppers-Lalic, F.J. Verweij, M. Pérez Lanzón, N. Zini, et al., Human bone marrow- and adipose-mesenchymal stem cells secrete exosomes enriched in distinctive miRNA and tRNA species, Stem Cell Res. Ther. 6 (2015) 1–20.
- T. Chen, R. Yeo, F. Arslan, Y. Yin, S. Tan, Efficiency of exosome production correlates inversely with the developmental maturity of MSC donor, J. Stem Cell Res. Ther. 3 (2013) 2.
- R.C. Lai, S.S. Tan, B.J. Teh, S.K. Sze, F. Arslan, D.P. de Kleijn, et al., Proteolytic potential of the MSC exosome proteome: implications for an exosome-mediated delivery of therapeutic proteasome, Int. J. Proteomics 2012 (2012) 971907.
- T.S. Chen, R.C. Lai, M.M. Lee, A.B.H. Choo, C.N. Lee, S.K. Lim, Mesenchymal stem cell secretes microparticles enriched in pre-microRNAs, Nucleic Acids Res. 38 (2010) 215–224.
- R.W. Yeo, R.C. Lai, K.H. Tan, S.K. Lim, Exosome: a novel and safer therapeutic refinement of mesenchymal stem cell, J. Circ. Biomark. 1 (2013) 7.
- R.C. Lai, R.W. Yeo, S.K. Lim, Mesenchymal stem cell exosomes, Semin. Cell Dev. Biol. 40 (2015) 82–88.
- B. Zhang, R.W. Yeo, K.H. Tan, S.K. Lim, Focus on extracellular vesicles: therapeutic potential of stem cell-derived extracellular vesicles, Int. J. Mol. Sci. 17 (2016) 174.
- Hu G-w, Q. Li, X. Niu, B. Hu, J. Liu, Zhou S-m, et al., Exosomes secreted by human-induced pluripotent stem cell-derived mesenchymal stem cells attenuate limb ischemia by promoting angiogenesis in mice, Stem Cell Res. Ther. 6 (2015) 1–15.
- J. Zhang, J. Guan, X. Niu, G. Hu, S. Guo, Q. Li, et al., Exosomes released from human induced pluripotent stem cells-derived MSCs facilitate cutaneous wound healing by promoting collagen synthesis and angiogenesis, J. Transl. Med. 13 (2015) 1–14.
- B. Zhang, M. Wang, A. Gong, X. Zhang, X. Wu, Y. Zhu, et al., HucMSC-exosome mediated-Wnt4 signaling is required for cutaneous wound healing, Stem Cells 33 (2015) 2158–2168.
- B. Zhang, Y. Yin, R.C. Lai, S.S. Tan, A.B.H. Choo, S.K. Lim, Mesenchymal stem cells secrete immunologically active exosomes, Stem Cells Dev. 23 (2013) 1233–1244.
- C.Y. Tan, R.C. Lai, W. Wong, Y.Y. Dan, S.-K. Lim, H.K. Ho, Mesenchymal stem cell-derived exosomes promote hepatic regeneration in drug-induced liver injury models, Stem Cell Res. Ther. 5 (2014) 1–14.
- C. Lee, S.A. Mitsialis, M. Aslam, S.H. Vitali, E. Vergadi, G. Konstantinou, et al., Exosomes mediate the cytoprotective action of mesenchymal stromal cells on hypoxia-induced pulmonary hypertension, Circulation 126 (2012) 2601–2611.
- B. Yu, H. Shao, C. Su, Y. Jiang, X. Chen, L. Bai, et al., Exosomes derived from MSCs ameliorate retinal laser injury partially by inhibition of MCP-1, Sci. Rep. 6 (2016) 34562.
- Jo CH, Lee YG, Shin WH, et al. Intra-articular injection of mesenchymal stem cells for the treatment of osteoarthritis of the knee: a proof of concept clinical trial. Stem Cells. 2014;32(5):1254–66.
- Vega, Aurelio, et al. Treatment of knee osteoarthritis with allogeneic bone marrow mesenchymal stem cells: a randomized controlled trial. Transplantation. 2015;99(8):1681–90.
- Davatchi F, Sadeghi-Abdollahi B, Mohyeddin M, et al. Mesenchymal stem cell therapy for knee osteoarthritis. Preliminary report of four patients. Int J Rheum Dis. 2011;14(2):211–5
- Hernigou P, Flouzat Lachaniette CH, Delambre J, et al. Biologic augmentation of rotator cuff repair with mesenchymal stem cells during arthroscopy improves healing and prevents further tears: a case- controlled study. Int Orthop. 2014;38(9):1811–1818
- Galli D, Vitale M, Vaccarezza M. Bone marrow-derived mesenchymal cell differentiation toward myogenic lineages: facts and perspectives. Biomed Res Int. 2014;2014:6.
- Beitzel K, Solovyova O, Cote MP, et al. The future role of mesenchymal Stem cells in The management of shoulder disorders. Arthroscopy. 2013;29(10):1702–1711.
- Isaac C, Gharaibeh B, Witt M, Wright VJ, Huard J. Biologic approaches to enhance rotator cuff healing after injury. J Shoulder Elbow Surg. 2012;21(2):181–190.
- Malda, Jos, et al. "Extracellular vesicles [mdash] new tool for joint repair and regeneration." Nature Reviews Rheumatology (2016).
Further References for MSC, BMC, Stemcell Secretome and EVs
- Georg Hansmann, Philippe Chouvarine, Franziska Diekmann, Martin Giera, Markus Ralser, Michael Mülleder, Constantin von Kaisenberg, Harald Bertram, Ekaterina Legchenko & Ralf Hass "Human umbilical cord mesenchymal stem cell-derived treatment of severe pulmonary arterial hypertension". Nature Cardiovascular Research volume 1, pages568–576 (2022).
- Murphy JM, Fink DJ, Hunziker EB, et al. Stem cell therapy in a caprine model of osteoarthritis . Arthritis Rheum. 2003;48:3464–74.
- Lee KB, Hui JH, Song IC, Ardany L, et al. Injectable mesenchymal stem cell therapy for large cartilage defects—a porcine model. Stem Cell. 2007;25:2964–71.
- Saw KY, Hussin P, Loke SC, et al. Articular cartilage regeneration with autologous marrow aspirate and hyaluronic acid: an experimental study in a goat model. Arthroscopy . 2009;25(12):1391–400.
- Black L, Gaynor J, Adams C, et al. Effect of intra-articular injection of autologous adipose-derived mesenchymal stem and regenerative cells on clinical signs of chronic osteoarthritis of the elbow joint in dogs. Vet Ther. 2008;9:192-200.
- Centeno C, Busse D, Kisiday J, et al. Increased knee cartilage volume in degenerative joint disease using percutaneously implanted, autologous mesenchymal stem cells. Pain Physician. 2008;11(3):343–53.
- Centeno C, Kisiday J, Freeman M, et al. Partial regeneration of the human hip via autologous bone marrow nucleated cell transfer: a case study. Pain Physician. 2006;9:253–6.
- Centeno C, Schultz J, Cheever M. Safety and complications reporting on the re-implantation of culture-expanded mesenchymal stem cells using autologous platelet lysate technique. Curr Stem Cell. 2011;5(1):81–93.
- Pak J. Regeneration of human bones in hip osteonecrosis and human cartilage in knee osteoarthritis with autologous adipose derived stem cells: a case series. J Med Case Rep. 2001;5:296.
- Kuroda R, Ishida K, et al. Treatment of a full-thickness articular cartilage defect in the femoral condyle of an athlete with autologous bone-marrow stromal cells. Osteoarthritis Cartilage. 2007;15:226–31.
- Emadedin M, Aghdami N, Taghiyar L, et al. Intra-articular injection of autologous mesenchymal stem cells in six patients with knee osteoarthritis. Arch Iran Med. 2012;15(7):422–8.
- Saw KY et al. Articular cartilage regeneration with autologous peripheral blood stem cells versus hyaluronic acid: a randomized controlled trial. Arthroscopy. 2013;29(4):684–94.
- Vangsness CT, Farr J, Boyd J, et al. Adult human mesenchymal stem cells delivered via intra-articular injection to the knee following partial medial meniscectomy. J Bone Joint Surg. 2014;96(2):90–8.
- Freitag, Julien, et al. Mesenchymal stem cell therapy in the treatment of osteoarthritis: reparative pathways, safety and efficacy–a review. BMC musculoskeletal disorders 17.1 (2016): 230.
- Maumus, Marie, Christian Jorgensen, and Danièle Noël. " Mesenchymal stem cells in regenerative medicine applied to rheumatic diseases: role of secretome and exosomes. " Biochimie 95.12 (2013): 2229-2234.
- Dostert, Gabriel, et al. " How do mesenchymal stem cells influence or are influenced by microenvironment through extracellular vesicles communication?. " Frontiers in Cell and Developmental Biology 5 (2017).
- Chaparro, Orlando, and Itali Linero. " Regenerative Medicine: A New Paradigm in Bone Regeneration. " (2016).
- Toh, Wei Seong, et al. " MSC exosome as a cell-free MSC therapy for cartilage regeneration: Implications for osteoarthritis treatment. " Seminars in Cell & Developmental Biology. Academic Press, 2016.
- Chaparro, Orlando, and Itali Linero. " Regenerative Medicine: A New Paradigm in Bone Regeneration. " (2016).
- S. Koelling, J. Kruegel, M. Irmer, J.R. Path, B. Sadowski, X. Miro, et al., Migratory chondrogenic progenitor cells from repair tissue during the later stages of human osteoarthritis , Cell Stem Cell 4 (2009) 324–335.
- B.A. Jones, M. Pei, Synovium-Derived stem cells: a tissue-Specific stem cell for cartilage engineering and regeneration , Tissue Eng. B: Rev. 18 (2012) 301–311.
- W. Ando, J.J. Kutcher, R. Krawetz, A. Sen, N. Nakamura, C.B. Frank, et al., Clonal analysis of synovial fluid stem cells to characterize and identify stable mesenchymal stromal cell/mesenchymal progenitor cell phenotypes in a porcine model: a cell source with enhanced commitment to the chondrogenic lineage, Cytotherapy 16 (2014) 776–788.
- K.B.L. Lee, J.H.P. Hui, I.C. Song, L. Ardany, E.H. Lee, Injectable mesenchymal stem cell therapy for large cartilage defects—a porcine model, Stem Cells 25 (2007) 2964–2971.
- W.-L. Fu, C.-Y. Zhou, J.-K. Yu, A new source of mesenchymal stem cells for articular cartilage repair: mSCs derived from mobilized peripheral blood share similar biological characteristics in vitro and chondrogenesis in vivo as MSCs from bone marrow in a rabbit model , Am. J. Sports Med. 42 (2014) 592–601.
- X. Xie, Y. Wang, C. Zhao, S. Guo, S. Liu, W. Jia, et al., Comparative evaluation of MSCs from bone marrow and adipose tissue seeded in PRP-derived scaffold for cartilage regeneration , Biomaterials 33 (2012) 7008–7018.
- E.-R. Chiang, H.-L. Ma, J.-P. Wang, C.-L. Liu, T.-H. Chen, S.-C. Hung, Allogeneic mesenchymal stem cells in combination with hyaluronic acid for the treatment of osteoarthritis in rabbits , PLoS One 11 (2016) e0149835.
- H. Nejadnik, J.H. Hui, E.P. Feng Choong, B.-C. Tai, E.H. Lee, Autologous bone marrow–derived mesenchymal stem cells versus autologous chondrocyte implantation: an observational cohort study , Am. J. Sports Med. 38 (2010) 1110–1116.
- I. Sekiya, T. Muneta, M. Horie, H. Koga, Arthroscopic transplantation of synovial stem cells improves clinical outcomes in knees with cartilage defects , Clin. Orthop. Rel. Res. 473 (2015) 2316–2326.
- Y.S. Kim, Y.J. Choi, Y.G. Koh, Mesenchymal stem cell implantation in knee osteoarthritis: an assessment of the factors influencing clinical outcomes , Am. J. Sports Med. 43 (2015) 2293–2301.
- W.-L. Fu, Y.-F. Ao, X.-Y. Ke, Z.-Z. Zheng, X. Gong, D. Jiang, et al., Repair of large full-thickness cartilage defect by activating endogenous peripheral blood stem cells and autologous periosteum flap transplantation combined with patellofemoral realignment , Knee 21 (2014) 609–612.
- Y.-G. Koh, O.-R. Kwon, Y.-S. Kim, Y.-J. Choi, D.-H. Tak, Adipose-derived mesenchymal stem cells with microfracture versus microfracture alone: 2-year follow-up of a prospective randomized trial , Arthrosc. J. Arthrosc. Relat. Surg. 32 (2016) 97–109.
- T.S. de Windt, L.A. Vonk, I.C.M. Slaper-Cortenbach, M.P.H. van den Broek, R. Nizak, M.H.P. van Rijen, et al., Allogeneic mesenchymal stem cells stimulate cartilage regeneration and are safe for single-Stage cartilage repair in humans upon mixture with recycled autologous chondrons , Stem Cells (2016) (n/a-n/a).
- L. da Silva Meirelles, A.M. Fontes, D.T. Covas, A.I. Caplan, Mechanisms involved in the therapeutic properties of mesenchymal stem cells , Cytokine Growth Factor Rev. 20 (2009) 419–427.
- W.S. Toh, C.B. Foldager, M. Pei, J.H.P. Hui, Advances in mesenchymal stem cell-based strategies for cartilage repair and regeneration , Stem Cell Rev. Rep. 10 (2014) 686–696.
- R.C. Lai, F. Arslan, M.M. Lee, N.S.K. Sze, A. Choo, T.S. Chen, et al., Exosome secreted by MSC reduces myocardial ischemia/reperfusion injury , Stem Cell Res. 4 (2010) 214–222.
- S. Zhang, W.C. Chu, R.C. Lai, S.K. Lim, J.H.P. Hui, W.S. Toh, Exosomes derived from human embryonic mesenchymal stem cells promote osteochondral regeneration, Osteoarthr . Cartil. 24 (2016) 2135–2140.
- S. Zhang, W. Chu, R. Lai, J. Hui, E. Lee, S. Lim, et al., 21 – human mesenchymal stem cell-derived exosomes promote orderly cartilage regeneration in an immunocompetent rat osteochondral defect model , Cytotherapy 18 (2016) S13.
- C.T. Lim, X. Ren, M.H. Afizah, S. Tarigan-Panjaitan, Z. Yang, Y. Wu, et al., Repair of osteochondral defects with rehydrated freeze-dried oligo[poly(ethylene glycol) fumarate] hydrogels seeded with bone marrow mesenchymal stem cells in a porcine model
- A. Gobbi, G. Karnatzikos, S.R. Sankineani, One-step surgery with multipotent stem cells for the treatment of large full-thickness chondral defects of the knee , Am. J. Sports Med. 42 (2014) 648–657.
- A. Gobbi, C. Scotti, G. Karnatzikos, A. Mudhigere, M. Castro, G.M. Peretti, One-step surgery with multipotent stem cells and Hyaluronan-based scaffold for the treatment of full-thickness chondral defects of the knee in patients older than 45 years , Knee Surg. Sports Traumatol. Arthrosc. (2016) 1–8.
- A. Gobbi, G. Karnatzikos, C. Scotti, V. Mahajan, L. Mazzucco, B. Grigolo, One-step cartilage repair with bone marrow aspirate concentrated cells and collagen matrix in full-thickness knee cartilage lesions: results at 2-Year follow-up , Cartilage 2 (2011) 286–299.
- K.L. Wong, K.B.L. Lee, B.C. Tai, P. Law, E.H. Lee, J.H.P. Hui, Injectable cultured bone marrow-derived mesenchymal stem cells in varus knees with cartilage defects undergoing high tibial osteotomy: a prospective, randomized controlled clinical trial with 2 years’ follow-up , Arthrosc. J. Arthrosc. Relat. Surg. 29 (2013) 2020–2028.
- J.M. Hare, J.E. Fishman, G. Gerstenblith, et al., Comparison of allogeneic vs autologous bone marrow–derived mesenchymal stem cells delivered by transendocardial injection in patients with ischemic cardiomyopathy: the poseidon randomized trial, JAMA 308 (2012) 2369–2379.
- L. Wu, J.C.H. Leijten, N. Georgi, J.N. Post, C.A. van Blitterswijk, M. Karperien, Trophic effects of mesenchymal stem cells increase chondrocyte proliferation and matrix formation , Tissue Eng. A 17 (2011) 1425–1436.
- L. Wu, H.-J. Prins, M.N. Helder, C.A. van Blitterswijk, M. Karperien, Trophic effects of mesenchymal stem cells in chondrocyte Co-Cultures are independent of culture conditions and cell sources , Tissue Eng. A 18 (2012) 1542–1551.
- S.K. Sze, D.P.V. de Kleijn, R.C. Lai, E. Khia Way Tan, H. Zhao, K.S. Yeo, et al., Elucidating the secretion proteome of human embryonic stem cell-derived mesenchymal stem cells , Mol. Cell. Proteomics 6 (2007) 1680–1689.
- M.B. Murphy, K. Moncivais, A.I. Caplan, Mesenchymal stem cells: environmentally responsive therapeutics for regenerative medicine , Exp. Mol. Med. 45 (2013) e54.
- M.J. Lee, J. Kim, M.Y. Kim, Y.-S. Bae, S.H. Ryu, T.G. Lee, et al., Proteomic analysis of tumor necrosis factor--induced secretome of human adipose tissue-derived mesenchymal stem cells , J. Proteome Res. 9 (2010) 1754–1762.
- S. Bruno, C. Grange, M.C. Deregibus, R.A. Calogero, S. Saviozzi, F. Collino, et al., Mesenchymal stem cell-derived microvesicles protect against acute tubular injury, J. Am. Soc. Nephrol. 20 (2009) 1053–1067.
- M. Yá˜nez-Mó, P.R.-M. Siljander, Z. Andreu, A.B. Zavec, F.E. Borràs, E.I. Buzas, et al. Biological properties of extracellular vesicles and their physiological functions (2015).
- C. Lawson, J.M. Vicencio, D.M. Yellon, S.M. Davidson, Microvesicles and exosomes: new players in metabolic and cardiovascular disease , J. Endocrinol. 228 (2016) R57–R71.
- A.G. Thompson, E. Gray, S.M. Heman-Ackah, I. Mager, K. Talbot, S.E. Andaloussi, et al., Extracellular vesicles in neurodegenerative diseas—pathogenesis to biomarkers, Nat. Rev. Neurol. 12 (2016) 346–357.
- I.E.M. Bank, L. Timmers, C.M. Gijsberts, Y.-N. Zhang, A. Mosterd, J.-W. Wang, et al., The diagnostic and prognostic potential of plasma extracellular vesicles for cardiovascular disease , Expert Rev. Mol. Diagn. 15 (2015) 1577–1588.
- T. Kato, S. Miyaki, H. Ishitobi, Y. Nakamura, T. Nakasa, M.K. Lotz, et al., Exosomes from IL-1 stimulated synovial fibroblasts induce osteoarthritic changes in articular chondrocytes , Arthritis. Res. Ther. 16 (2014) 1–11.
- R.W.Y. Yeo, S.K. Lim, Exosomes and their therapeutic applications, in: C. Gunther, A. Hauser, R. Huss (Eds.), Advances in Pharmaceutical Cell TherapyPrinciples of Cell-Based Biopharmaceuticals, World Scientific, Singapore, 2015, pp. 477–491.
- X. Qi, J. Zhang, H. Yuan, Z. Xu, Q. Li, X. Niu, et al., Exosomes secreted by human-Induced pluripotent stem cell-derived mesenchymal stem cells repair critical-sized bone defects through enhanced angiogenesis and osteogenesis in osteoporotic rats , Int. J. Biol. Sci. 12 (2016) 836–849.
- R.C. Lai, F. Arslan, S.S. Tan, B. Tan, A. Choo, M.M. Lee, et al., Derivation and characterization of human fetal MSCs: an alternative cell source for large-scale production of cardioprotective microparticles , J. Mol. Cell. Cardiol. 48 (2010) 1215–1224.
- Y. Zhou, H. Xu, W. Xu, B. Wang, H. Wu, Y. Tao, et al., Exosomes released by human umbilical cord mesenchymal stem cells protect against cisplatin-induced renal oxidative stress and apoptosis in vivo and in vitro , Stem Cell Res. Ther. 4 (2013) 1–13.
- Y. Qin, L. Wang, Z. Gao, G. Chen, C. Zhang, Bone marrow stromal/stem cell-derived extracellular vesicles regulate osteoblast activity and differentiation in vitro and promote bone regeneration in vivo , Sci. Rep. 6 (2016) 21961.
- M. Nakano, K. Nagaishi, N. Konari, Y. Saito, T. Chikenji, Y. Mizue, et al., Bone marrow-derived mesenchymal stem cells improve diabetes-induced cognitive impairment by exosome transfer into damaged neurons and astrocytes , Sci. Rep. 6 (2016) 24805.
- K. Nagaishi, Y. Mizue, T. Chikenji, M. Otani, M. Nakano, N. Konari, et al., Mesenchymal stem cell therapy ameliorates diabetic nephropathy via the paracrine effect of renal trophic factors including exosomes , Sci. Rep. 6 (2016) 34842.
- S.R. Baglio, K. Rooijers, D. Koppers-Lalic, F.J. Verweij, M. Pérez Lanzón, N. Zini, et al., Human bone marrow- and adipose-mesenchymal stem cells secrete exosomes enriched in distinctive miRNA and tRNA species , Stem Cell Res. Ther. 6 (2015) 1–20.
- T. Chen, R. Yeo, F. Arslan, Y. Yin, S. Tan, Efficiency of exosome production correlates inversely with the developmental maturity of MSC donor, J. Stem Cell Res. Ther. 3 (2013) 2.
- R.C. Lai, S.S. Tan, B.J. Teh, S.K. Sze, F. Arslan, D.P. de Kleijn, et al., Proteolytic potential of the MSC exosome proteome: implications for an exosome-mediated delivery of therapeutic proteasome , Int. J. Proteomics 2012 (2012) 971907.
- T.S. Chen, R.C. Lai, M.M. Lee, A.B.H. Choo, C.N. Lee, S.K. Lim, Mesenchymal stem cell secretes microparticles enriched in pre-microRNAs , Nucleic Acids Res. 38 (2010) 215–224.
- R.W. Yeo, R.C. Lai, K.H. Tan, S.K. Lim, Exosome: a novel and safer therapeutic refinement of mesenchymal stem cell, J. Circ. Biomark. 1 (2013) 7.
- R.C. Lai, R.W. Yeo, S.K. Lim, Mesenchymal stem cell exosomes, Semin. Cell Dev. Biol. 40 (2015) 82–88.
- B. Zhang, R.W. Yeo, K.H. Tan, S.K. Lim, Focus on extracellular vesicles: therapeutic potential of stem cell-derived extracellular vesicles , Int. J. Mol. Sci. 17 (2016) 174.
- Hu G-w, Q. Li, X. Niu, B. Hu, J. Liu, Zhou S-m, et al., Exosomes secreted by human-induced pluripotent stem cell-derived mesenchymal stem cells attenuate limb ischemia by promoting angiogenesis in mice , Stem Cell Res. Ther. 6 (2015) 1–15.
- J. Zhang, J. Guan, X. Niu, G. Hu, S. Guo, Q. Li, et al., Exosomes released from human induced pluripotent stem cells-derived MSCs facilitate cutaneous wound healing by promoting collagen synthesis and angiogenesis , J. Transl. Med. 13 (2015) 1–14.
- B. Zhang, M. Wang, A. Gong, X. Zhang, X. Wu, Y. Zhu, et al., HucMSC-exosome mediated-Wnt4 signaling is required for cutaneous wound healing, Stem Cells 33 (2015) 2158–2168.
- B. Zhang, Y. Yin, R.C. Lai, S.S. Tan, A.B.H. Choo, S.K. Lim, Mesenchymal stem cells secrete immunologically active exosomes , Stem Cells Dev. 23 (2013) 1233–1244.
- C.Y. Tan, R.C. Lai, W. Wong, Y.Y. Dan, S.-K. Lim, H.K. Ho, Mesenchymal stem cell-derived exosomes promote hepatic regeneration in drug-induced liver injury models , Stem Cell Res. Ther. 5 (2014) 1–14.
- C. Lee, S.A. Mitsialis, M. Aslam, S.H. Vitali, E. Vergadi, G. Konstantinou, et al., Exosomes mediate the cytoprotective action of mesenchymal stromal cells on hypoxia-induced pulmonary hypertension , Circulation 126 (2012) 2601–2611.
- B. Yu, H. Shao, C. Su, Y. Jiang, X. Chen, L. Bai, et al., Exosomes derived from MSCs ameliorate retinal laser injury partially by inhibition of MCP-1 , Sci. Rep. 6 (2016) 34562.
- Jo CH, Lee YG, Shin WH, et al. Intra-articular injection of mesenchymal stem cells for the treatment of osteoarthritis of the knee: a proof of concept clinical trial. Stem Cells. 2014;32(5):1254–66.
- Vega, Aurelio, et al. Treatment of knee osteoarthritis with allogeneic bone marrow mesenchymal stem cells: a randomized controlled trial. Transplantation. 2015;99(8):1681–90.
- Davatchi F, Sadeghi-Abdollahi B, Mohyeddin M, et al. Mesenchymal stem cell therapy for knee osteoarthritis. Preliminary report of four patients. Int J Rheum Dis. 2011;14(2):211–5
- Hernigou P, Flouzat Lachaniette CH, Delambre J, et al. Biologic augmentation of rotator cuff repair with mesenchymal stem cells during arthroscopy improves healing and prevents further tears: a case- controlled study. Int Orthop. 2014;38(9):1811–1818
- Galli D, Vitale M, Vaccarezza M. Bone marrow-derived mesenchymal cell differentiation toward myogenic lineages: facts and perspectives. Biomed Res Int. 2014;2014:6.
- Beitzel K, Solovyova O, Cote MP, et al. The future role of mesenchymal Stem cells in The management of shoulder disorders . Arthroscopy. 2013;29(10):1702–1711.
- Isaac C, Gharaibeh B, Witt M, Wright VJ, Huard J. Biologic approaches to enhance rotator cuff healing after injury. J Shoulder Elbow Surg. 2012;21(2):181–190.
- Malda, Jos, et al. " Extracellular vesicles [mdash] new tool for joint repair and regeneration. " Nature Reviews Rheumatology (2016).
Further References about PRP
- Rubio-Azpeitia E, Andia I. Partnership between platelet-rich plasma and mesenchymal stem cells: in vitro experience. Muscles Ligaments Tendons J. 2014;4(1):52–62.
Extras
- Xu, Ming, et al. " Transplanted senescent cells induce an osteoarthritis-like condition in mice. " The Journals of Gerontology Series A: Biological Sciences and Medical Sciences (2016): glw154.
- McCulloch, Kendal, Gary J. Litherland, and Taranjit Singh Rai. " Cellular senescence in osteoarthritis pathology ." Aging Cell (2017).
Patient Services at ANOVA Institute for Regenerative Medicine
- Located in the center of Germany, quick access by car or train from anywhere in Europe
- Simple access worldwide, less than 20 minutes from Frankfurt Airport
- Individualized therapy with state-of-the-art stem cell products
- Individually planned diagnostic work-up which include world-class MRI and CT scans
- German high quality standard on safety and quality assurance
- Personal service with friendly, dedicated Patient Care Managers
- Scientific collaborations with academic institutions to assure you the latest regenerative medical programs